Seven ideas to reduce the environmental impact of point-of-care diagnostics
By Elena Boland

Point-of-care diagnostic tests offer speed and convenience to healthcare providers and patients alike. But the vast majority of test kits and cartridges are currently designed to be disposable, so manufacturers need to be ready to make near-patient and at-home diagnostics with lower environmental impact. We look at some ideas to reduce, eliminate or even use more single-use plastics in the interest of sustainability.
During the COVID-19 pandemic, how many of us felt a twinge of guilt as we threw our single-use lateral flow tests into the household waste?
Single use point-of-care diagnostics relying heavily on plastic consumables and cartridges are becoming more popular in clinical settings, where they enable faster turnaround times and better patient outcomes.
To add to that, there is an increasing trend towards shifting more and more healthcare into patients’ homes. This can save costs and is generally better for patients, but nevertheless increases the number of diagnostic devices and associated plastic waste.
The expansion of distributed healthcare and increasing demands for sustainability – from patients, providers and regulators – mean that it’s now time to be far more ambitious in developing sustainable point-of-care diagnostics.
At TTP, we think it’s best to consider these ideas early in product development because this is when you can consider all the trade-offs and take unconstrained decisions to meet your goals.

1. Consider more sustainable plastics
While there may be a temptation to work with plastics you’re familiar with, stepping outside of this “comfort zone” to trial more sustainable plastics is definitely something to consider.
The three main options are:
- Recycled plastics contribute to the development of a “circular economy” for plastics. In clinical applications, their use may prompt questions about material quality and uniformity, but experienced product designers will be able to negotiate these through careful material selection and device architecture design.
- Bio-based plastics (or “bioplastics”) originate at least in part from renewable feedstocks, such as corn starch, sugarcane, vegetable oils or agricultural waste, and so can avoid reliance on fossil-based sources.
- Biodegradable plastics can break down under the right conditions and can help to divert waste streams away from landfill and/or reduce long-term pollution from incorrect disposal.
The number of options in this area is rapidly increasing, making it ever easier to meet device performance requirements, prototyping needs and eventual manufacturing processes with improved sustainability in mind.
2. Minimise the use of virgin or fossil-based plastics
Sometimes only virgin and/or fossil-based polymers will give the necessary tolerances in the finished product or the required surface properties. If so, your next option is to reduce the amount of these types of plastics.
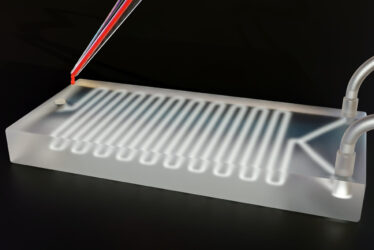
To take a microfluidic testing device as an example, the fluid path in contact with the human sample may need to be virgin plastic. But the parts that are there simply to provide rigidity may be made of more sustainable plastics, or even non-plastic materials.
At TTP, we’ve recently created ecoflex, a low-cost sample-to-answer ELISA system that delivers central-lab performance but restricts plastic material use to the parts in contact with the sample and uses structural components derived from paper pulp.

3. Remember that “small is beautiful”
One of the best ways to make a product more sustainable is through miniaturisation – essentially making the amount of material used as small as possible.
However, the device still needs to be reliable, whoever is using it. In the case of near-patient devices, this could be anyone from a busy nurse in a hospital ward, to a parent worried about the health of their child.
In fact, this ability to give reliable results in the hands of “unskilled operators” is something that regulators place great emphasis on, as embodied by the CLIA waiver applied in the US to tests that are simple enough for non-lab use. Designers specialising in human factors can ensure that the sustainability considerations are balanced with ease of use.

4. Expand end-of-life disposal routes open to your product
In healthcare settings, incineration of clinical waste streams is common to deal with materials that pose a biological or chemical hazard. If test reagents were developed to be safer, and test systems designed to inactivate any potential biohazards, more environmentally friendly disposal options may become available.
This point is well worth considering, because although it’s currently acceptable to ask users to dispose of devices “in accordance with local rules”, this may change as manufacturers are obliged to take more responsibility for the environmental impact of their products. For example, if the disposal route is impractical or costly, manufacturers may be forced to collect devices, and bear the burden of specialised disposal themselves. So, it’s worth improving the end-of-life disposal routes available to your product.

5. Consider instrument and assay development as one
Traditionally, most in vitro diagnostic assays are developed by bioscientists working with standard lab equipment. Only after that do engineers and designers work out how to transfer the assay to a test cartridge. This process often requires work-arounds to replace the operations previously carried out by hand. This can easily lead to “over-engineering” and consequent over-use of materials.
Ideally, bioscientists, engineers and designers should work together from the outset to create a test that works most efficiently for its intended purpose. To this end, TTP is developing modular tools that can be quickly adapted to support assay development and enable you to create the final assay with the minimum number of adaptations.

6. Investigate cartridge-free options
Can we design point-of-care diagnostic platforms to work without disposable cartridges?
Clearly, the parts of the device that come into contact with the patient sample would need to be flushed (or otherwise treated) to make them ready for the next sample. But if that could be achieved, only liquid waste would be generated.
This liquid waste may then need to be made safe for disposal, but this may be more sustainable than a single use of a test kit, particularly if the system was designed with safer chemicals and decontamination routes in mind.
This concept is not without its difficulties. In diagnostic devices, there may be a risk of contaminating a subsequent sample or loss of test performance due to inadequate cleaning. But with rigorous device design and validation of cleaning methods – similar to that employed for GMP purposes in pharma – it should be possible to demonstrate that cross-contamination is highly unlikely.

7. Take a wider view
So far, we’ve focused on reducing the direct environmental impact of point-of-care or at-home diagnostics. However, it’s worth looking at the bigger picture as well, especially when the impact of a test cannot be reduced as much as might be desired.
For example, carrying out a blood test at home should be contrasted with the alternative – visiting a hospital to give a sample that is then sent off to a central lab. This conventional route may involve:
- Carbon emissions from the patient traveling to and from hospital
- Increased risk of transmitting infections within the hospital, and the carbon and resource impact of others becoming ill
- Use of plastics to transport and secure samples between the hospital and the central lab
- Consumables used at the central lab (e.g., assay plates and pipette tips)
Set in this context, a finger-prick test performed in the patient’s own home on a device that incorporates some of the ideas mentioned above may well offer a much better sustainability profile, even if the use of single-use plastic is unavoidable – or indeed desirable to improve the likelihood that the test will be used correctly by the patient and realises the sustainability “co-benefits” outlined above.
Making tests more sustainable by design
There is great potential for point-of-care and at-home assays to offer streamlined testing and laboratory-quality results, with all the improvements for healthcare that follow from that. But as these tests grow in popularity, manufacturers must not lose sight of growing demand for improving the sustainability of all products, especially those that use plastic.
Need some guidance on making your point-of-care test kit more sustainable? Give us a call today to talk to one of our experts.



